A bipartisan group of eight senators unveiled legislation Tuesday that addresses an opioid epidemic that killed nearly 64,000 people in 2016 alone and shortened life expectancy by about three months.
CARA 2.0 — advertised as a sequel to the last major bill to address the opioid epidemic, the Comprehensive Addiction and Recovery Act of late 2016 — would impose new rules to prescribing opioids and dedicate $1 billion to addiction treatment and recovery programs. The bill adds money to existing and new programs, and pitches six new policies, including a three-day limit on prescription opioids for acute pain and increased criminal and civil penalties for opioid manufacturers that don’t report suspicious orders.
If passed, this would be the most meaningful action from Congress since President Donald Trump took office and declared the opioid crisis a public health emergency. Still, it falls short of what’s needed to tackle the crisis.
Perhaps most notable is the measure allowing physician assistance (PA) and nurse practitioners (NP) to prescribe a form of medication-assisted treatment, buprenorphine, under the direction of a qualified physician. This was a provision in the original CARA, which allowed PAs and NPs to prescribe buprenorphine with no additional training and certification under the direction of a qualified physician for five years and is set to sunset in 2021. CARA 2.0 is aiming to remove the sunset clause.
Experts overwhelmingly agree addiction treatment should be a top priority when thinking about this epidemic. Currently, doctors must obtain a certification and waiver to prescribe buprenorphine or other medication-assisted treatment. Health experts, including those at the American Action Forum, say “this stipulation has become a hindrance to providing care” as demand outpaces supply. Allowing PAs and NPs to provide medication-assisted treatment could be a big help.
But for this particular measure to successfully work, state lawmakers also need to prioritize expanding access to treatment, which means addressing restrictive state scope-of-practice laws. There is a serious provider shortage nationwide, and there are roughly a dozen or so state laws that restrict what NAs and PAs can do, thus blunting the policy’s effect in many states. Twenty-eight states specifically prohibit NPs from prescribing this safe and highly effective drug unless it’s in collaboration with a doctor licensed to prescribe it, according to an analysis of state laws by the Pew Charitable Trusts in 2017.
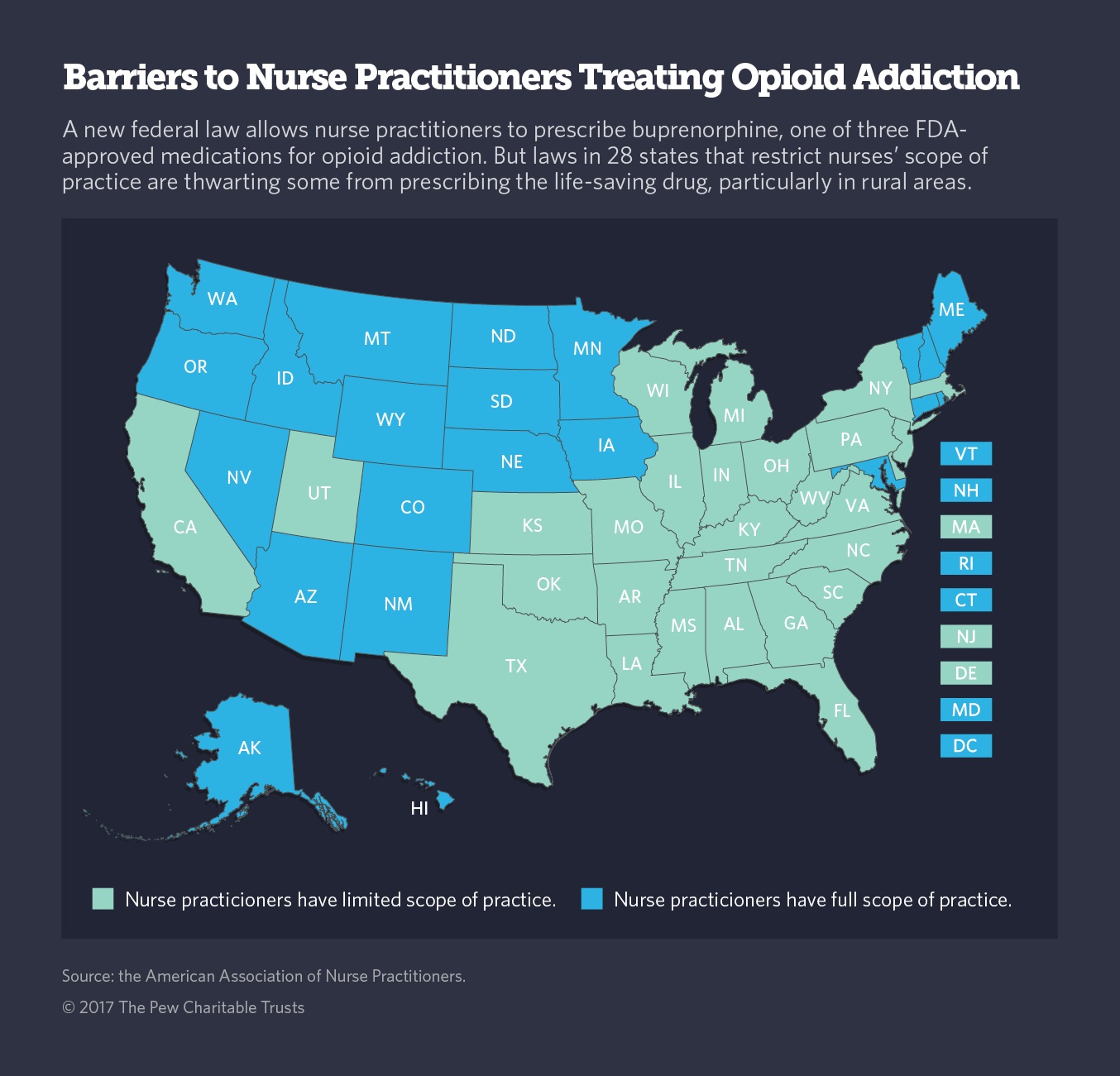
This presents a significant challenge for half of all counties in the United States that do not have a single licensed physician. Oklahoma, Tennessee, and Wyoming have laws explicitly prohibiting NPs from administering buprenorphine with or without a qualified doctor’s oversight. And in Kentucky, PAs are banned from providing buprenorphine. On the other hand, twenty-two states have expansive laws and allow nurse practitioners “full practice” — meaning, these medical workers can prescribe this type of drug independently of a qualified doctor.
A recent Avalere Health study compares how states are doing with providing addiction treatment and opioid overdose deaths, one way to measure rates of drug misuse. Researchers found the Midwest and Mid-Atlantic states face a serious provider shorter and, thus, have a harder time curbing the deadly epidemic.
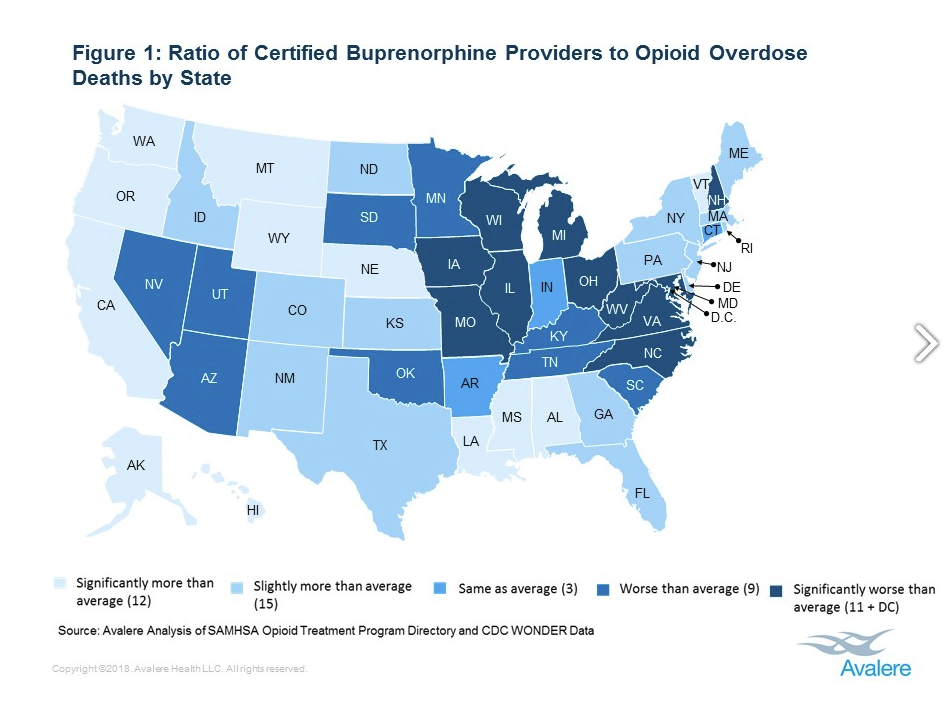
“Although more providers are now able to prescribe buprenorphine, there appears to be a shortage of prescribers in many states,” wrote Clara Soh, a director at Avalere. “Evaluating ways to narrow this gap, including bringing state scope-of-practice laws into alignment with federal regulations, would enable policymakers to achieve their goal to expand access.”
Federal law allows NAs and PAs to apply for licenses but some state laws prohibit them from applying. In an email to ThinkProgress, Soh explained CARA 2.0 would make the expansion for buprenorphine certification permanent, “mean[ing] that any states who allow NPs and PAs to prescribe buprenorphine-based MAT beyond Oct 2021 would not run afoul of federal laws, but the inverse would not automatically be true – states would still have to also allow these providers to prescribe buprenorphine.” Meaning, states need to act.
The bill also doesn’t address bigger issues in the health care system that are making it harder for people addicted to opioids to access the treatment they need. Congress spent most of the last year trying to repeal and replace the Affordable Care Act (ACA), which enables people with substance use disorder to get into treatment, and repealed the mandate which upholds the entire marketplace effective 2019. Also state officials across the country are seeking to implement work rules in their state Medicaid programs. Advocates fear people with substance use disorder could inadvertently drop coverage with all the added paperwork associated with new requirements.
UPDATE: This story has been updated to include how many states give nurse practitioners full practice authority.
